Editor’s note: This post is part of an ongoing series of posts featuring NCRP nonprofit members.
![]() Glenda Jimmo, a blind woman confined to a wheelchair after diabetes took her right leg, required multiple weekly home health services for her condition.
Glenda Jimmo, a blind woman confined to a wheelchair after diabetes took her right leg, required multiple weekly home health services for her condition.
A woman living with ALS who lost the user of her arms and hands required extensive care services in her home.
A World War II veteran stricken with Parkinson’s disease fell in his home and needed access to a skilled nursing facility for his recovery.
All three were denied Medicare coverage, the national health insurance program for which Social Security recipients who are over 65 or permanently disabled are eligible, because their conditions were “not improving” and thus not worthy of coverage.
Another woman was left helpless and alone after Medicare deemed her multiple sclerosis “not improving.” Bedridden and shut off from essential in-home nursing care, she went four days without food or water.
This “improvement standard” pervaded all of Medicare, informing the decisions of health care providers, contractors and even administrative law judges.
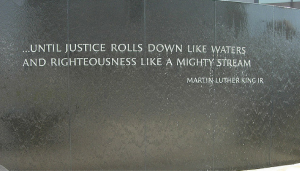
For decades, it was used to save money and deny coverage to the Americans who most direly needed care. But there was no regulation on the books that supported this practice. In fact, Medicare rules stipulate “the restoration potential of a patient is not the deciding factor in determining whether skilled services are needed.”
Put another way: The improvement standard was illegal. Medicare providers had conjured up a standard out of thin air, and to devastating effect.
The Center for Medicare Advocacy (CMA), a Connecticut-based organization that fights on behalf of older and disabled Americans to improve their access to and the quality of their health care, refused to abide this misguided practice.
Since its founding in 1986, CMA has taught Medicare administrators that the elderly and disabled need not show improvement to retain coverage if their current treatment is still the best way to care for them, e.g. if other options would lead to worse health outcomes.
This helped individual cases, but did little to stem the tide of wrongful coverage denials. Having exhausted all other advocacy options, CMA did what it had to do and took the federal government to court. They won.
This was literally a life-saving victory for people like Glenda Jimmo. And it’s not the first time CMA has used the courts to protect some of the most vulnerable among us.
The organization represents thousands of Americans in appeals of Medicare denials, and advocates on their behalf in administrative, executive and legal settings. Legal services have proven to be an effective arrow in the organization’s quiver.
But it’s only one arrow among many. Connecticut has contracted CMA to provide legal training and support for its health insurance and assistance program. CMA produces a host of educational materials and resources related to Medicare, and everyday Americans nationwide rely on CMA for expert Medicare information and insight.
In the National Medicare Advocates Alliance, CMA is joined by a network of attorneys, Medicare-related advocacy organizations and state health insurance providers for bimonthly conference calls on specific topics in Medicare, elders’ rights and elders’ health care.
The National Medicare Advocates Alliance began as a foundation-funded project more than a decade ago, but its national impact was so great that it felt compelled to continue the endeavor even after the original grants expired.
But the cost of managing CMA hasn’t gone away. Nor has the cost of fielding the hundreds of calls CMA receives each year from outside Connecticut when older or disabled Americans need expertise and counsel. Philanthropy has heretofore shown little interest in funding these services, and funders have been even more reticent to fund legal work, according to CMA.
The threats to Medicare access and quality continue to grow. CMA won an inspiring victory on the improvement standard, but that just pushed Medicare to enforce existing law correctly. Bigger, systemic perils like privatization of the program or a winding down of Medicare altogether endanger far more of our seniors and disabled.
Bigger, systemic problems require bigger, systemic solutions. Philanthropy needs to invest in long-term capacity so those working on this issue can build up the staffing necessary to hold the line on Medicare access and quality.
When they devise successful programs like the National Medicare Advocates Alliance, funders shouldn’t cut support after a year or two and ask for something new. Place the emphasis instead on enriching and broadening what has already proven to work.
Advocacy is a matter of using the best resources to tell the best stories in the best place possible. The Center for Medicare Advocacy has the stories and has the places. Imagine what they could do if they had the resources too.
Troy Price is NCRP’s membership and fundraising intern. Follow @NCRP on Twitter.






















































































































































































































































































































































































Leave a Reply